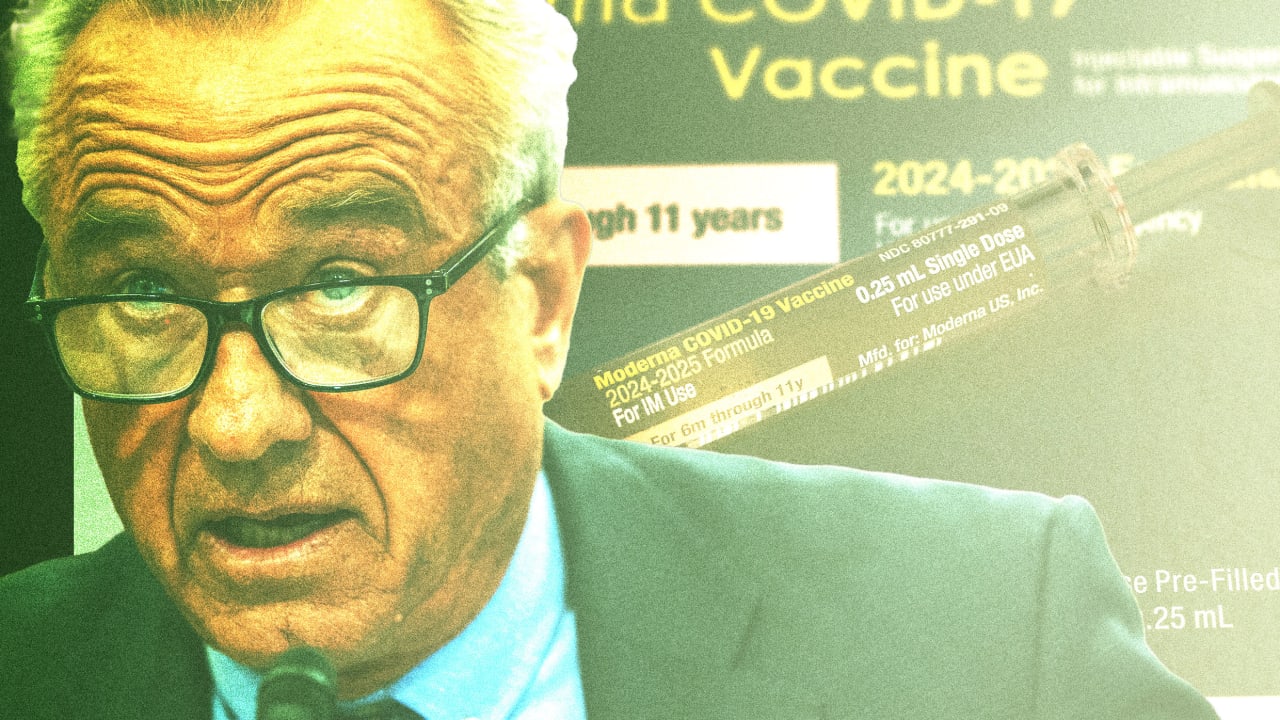
MAHA v. Moderna: The COVID vaccine maker is under attack by RFK Jr.’s department of health
Moderna CEO and cofounder Stéphane Bancel probably never imagined he’d look back on March 2023 as the good old days. Then, he merely had to go before the Senate Health, Education, Labor, and Pensions Committee and take a spitty dressing-down from Senator Bernie Sanders over the price of Moderna’s COVID vaccine. The company was held up as a poster child for “corporate greed.” For a U.S. pharma executive, though, that was more or less business as usual.
Today, the situation is anything but. With the confirmation of Robert F. Kennedy Jr., a prominent anti-vaxxer, to be the secretary of the Department of Health and Human Services this February, once-fringe medical theories have been escalated to the level of policy, throwing established scientific and regulatory norms into doubt. Among drugmakers, perhaps none is worse situated to absorb the D.C. vibe shift than Moderna, which is now being targeted not for its pricing but for its one and only product: mRNA-based vaccines.
Kennedy has shown a particular distaste for mRNA vaccines, such as those that were rapidly developed by Moderna and Pfizer-BioNTech in response to the global outbreak of COVID-19. During the height of the pandemic, Kennedy petitioned the Food and Drug Administration to revoke authorization for COVID-19 vaccines and not approve any future ones, saying that the risks of adverse reactions and death weren’t adequately studied. These vaccines—which have been safely administered to billions of people around the world and in 2021 alone saved at least an estimated 14.4 million lives worldwide—have been the subject of conspiracy theories and misinformation since they were first authorized for emergency use in late 2020. Among the debunked claims of critics: the vaccines can alter a person’s genome; they contain microchips or tracking devices; They cause something dubbed turbo cancer. Several states, including Florida, Kentucky, South Carolina, Idaho, and Texas are considering laws that would severely limit or ban the use of mRNA vaccines. Louisiana and Texas have already ended mass vaccinations and any promotion of the vaccines.
Now, Kennedy’s HHS is taking action against Moderna’s signature product. In the past month alone, the CDC has revised its public health recommendations for COVID-19 vaccines, the FDA altered its vaccine approval process, and the government canceled a $766 million contract with Moderna to develop new vaccines against pandemic threats including H5N1 avian influenza. Taken together, these moves have effectively knee-capped Moderna’s business. They’ve also jeopardized public health, and spread uncertainty across the burgeoning landscape of next-generation RNA-based therapeutics.
Moderna can ill afford an unfavorable regulatory environment, much less an administration seemingly bent on its destruction. The company, which declined to make executives available for this story, took in $3.2 billion last year—less than half of the year prior—at a net loss of $3.6 billion. For the first quarter this year, it brought in $100 million at a $1 billion loss. Although Moderna launched an RSV vaccine last year and is developing a personalized cancer immunotherapy, almost all of its money still comes from sales of COVID-19 shots, which are steadily declining. And with its entire technology under attack, Moderna’s future looks anything but certain.
Going all in on mRNA
While most pharma companies have grown by establishing franchises in particular diseases, Moderna has always been all-in on Bancel’s conception of a biotech “platform” company. The entire premise is right there in its ticker symbol: mRNA.
The promise of the technology is appealing. Older vaccines typically consist of weakened or killed viruses, or parts of viruses, to mimic an infection and elicit an immune response. These vaccines are grown in eggs or cell cultures, purified, and mixed with adjuvants that help them work in the body. Historically, developing vaccines in this way has taken anywhere from 5 to 10 years.
But mRNA vaccines don’t require any viruses, or eggs. Instead, they work by delivering into the body genetic “instructions,” in the form of mRNA molecules, that cells use to manufacture a protein called an antigen, which induces an immune response. The original COVID vaccine contained mRNA instructions to produce a signature “spike” protein found on the surface of the coronavirus.
Because mRNA is “digital”—like DNA, it encodes a series of nucleotide letters (A, U, G, C)—creating new mRNA vaccines is a relatively simple matter of rearranging these letters to create a different antigen. mRNA is made in an egg- and cell-free manufacturing process, and once the sequence for a vaccine has been selected, it can be manufactured in as little as a few weeks. This speed and flexibility are what enabled the development of a working vaccine for COVID within a year of its discovery. And it is why many experts in infectious disease believe mRNA vaccines are an essential tool in responding to future pandemic threats. Bancel has been banking on mRNA not only as a vaccine platform but also as a breakthrough way of treating cancer and other diseases.
Until last year, though, Moderna had brought just one product to the market: the Spikevax vaccine for COVID-19. In 2021, the company sold 807 million doses, pocketing $17.7 billion. The company’s stock soared—in 2021, Moderna’s market cap hovered around $200 billion, surpassing legacy drugmakers including GlaxoSmithKline, Amgen, and Merck. But demand for the vaccines has abated quickly. In 2022, Moderna had $18.4 billion in vaccine sales. In 2023, the year the public health emergency was declared over and the federal government phased out paying for the vaccine doses, Moderna’s sales were less than $7 billion. Last year, they more than halved yet again.
Moderna’s second commercial product, an mRNA vaccine for Respiratory Syncytial Virus (RSV) was approved by the FDA in May 2024, for people 60 years and older. Marketed as mRESVIA, it had total 2024 sales of $25 million. At the start of this year, Moderna’s stock was down about 90% from its pandemic peak. Moderna’s cash reserve, meanwhile, has dwindled from $18.2 billion at the end of 2022 to $8.4 billion today.
Last fall, Bancel announced a plan to cut R&D spending by $1.1 billion by 2027 and to shelve five early-stage programs. This January, he said at the JP Morgan Healthcare Conference that the company would cut $1 billion in spending this year alone, and find another $500 million in cuts next year.
As Moderna, which was founded in 2010, grew from 800 employees pre-pandemic to 5,600 full-time global employees at the end of 2023, it gained a reputation as a tough workplace that burned through talent. Even so, its recent departures have signaled a company in turmoil. Since late 2023, when chief commercial officer Arpa Garay left the company less than two years after joining from Merck, his former duties have been split between Bancel, covering sales and marketing, and Moderna’s president Stephen Hoge responsible for commercial pipeline strategy and medical affairs. In November 2024, Hoge took charge of sales, as well.
“Stephen and Stephane will go down with the ship,” says a former employee speaking on background. “They’re a $10 billion company now—how does that save them? They’re in a really bad position.” Others are jumping. This February, CIO Brad Miller—who’d been driving the company’s “tech-driven insights” for just over two years—“retired” at age 52, as Moderna downsized its digital departments by about 50 employees, or 10%. Pharma folks took notice in March, when Kate Cronin, who’d led marketing since 2021, left the company and a month later joined Medtronic Diabetes. “When Kate Cronin left, I thought, that’s the rat leaving the sinking ship,” says another industry insider. Multiple employees in communications roles have also recently left the company.
Keeping up with the FDA and CDC
Moderna’s pipeline includes vaccines for everything from shingles to HIV, as well as therapeutics for cancer and rare diseases. But near-term, its hopes had been riding on a new, improved COVID vaccine, along with a first-of-its-a-kind combination COVID-flu vaccine. In the last couple of weeks, though, those hopes have been tempered, if not crushed, by changes at the FDA and the Centers for Disease Control and Prevention, which taken together could dramatically limit who will get access to such vaccines moving forward—and determine whether companies like Moderna will continue to make them at all.
On May 31, Moderna had a partial win when the FDA approved its next-generation COVID-19 vaccine, called mNEXSPIKE. But unlike its predecessor, which is licensed for use for all individuals 12 years of age and older, regardless of health-risk status—it was authorized for use only for people aged 65 and older, or aged 12 to 64 with a qualifying medical condition. (The FDA’s delayed approval in May of a non-mRNA COVID vaccine made by Novavax had the same restrictions.) People aged 65 and older account for the majority of COVID vaccines, and benefit the most from their protection.
In previous years, as long as updated COVID shots showed evidence that they generated a comparable immune response to the previous year’s version, the FDA approved them for use for most people. Now, to get approval for anyone under 65 and without an underlying medical condition, vaccine makers will have to show additional safety and efficacy data from randomized controlled trials. (The FDA and its advisers had previously considered it unfeasible to run such trials quickly enough.) Calling for “robust, gold-standard data on persons at low risk,” the new requirements were put forth without the usual input from independent outside advisers.
Between 100 million to 200 million Americans (of a total population of 347 million) would be eligible for COVID vaccines under the new approach, according to an estimate cited by FDA commissioner Martin Makary and Vinay Prasad, director of the FDA’s Center for Biologics Evaluation and Research. But the changes in the approval process—as a new, highly transmissible COVID subvariant has been detected in California, heightening the risk of a summer wave—could leave a lot of people unprotected in the 2025–2026 season. On June 3, Kennedy announced on X that Moderna had “agreed to a true placebo-controlled trial” of the new vaccine; it’s not yet clear how that will impact availability of the 2025–2026 vaccine. Moderna declined to comment in response to Kennedy’s statement on X.
Further clouding the vaccination landscape is new CDC guidance about who should get an annual COVID booster. On May 28, Kennedy announced he was rescinding the government’s recommendation that pregnant women and healthy children get COVID immunizations. Without this recommendation, health insurers—including Medicaid—will not likely cover the cost of the vaccine. A couple of days later, the CDC partially contradicted Kennedy, advising that kids continue to get the vaccine—but only in consultation with a healthcare provider. It offered no additional guidance for pregnant women, who have higher risk for health complications from COVID.
Meanwhile, Moderna has voluntarily withdrawn its application for approval of its new combo flu/COVID vaccine after the FDA requested more efficacy data. Moderna expects to have additional data this summer, but it declined to share a target date for resubmitting its application.
Shutting down avian flu research
Perhaps the biggest recent blow to Moderna’s prospects came last week, when the U.S. Department of Health and Human Services terminated a contract with the company to develop vaccines against several strains of flu with pandemic potential, including the highly pathogenic avian flu viruses H1N1 and H7N9. Moderna had won the contract—originally worth $176 million but expanded in the last days of the Biden administration by another $590 million—on the belief that mRNA vaccines would be a critical part of any future pandemic response. Andrew Nixon, director of communications at HHS, told STAT that the agency had ended the contract because “continued investment in Moderna’s H5N1 mRNA vaccine was not scientifically or ethically justifiable.”
The same day that news came out, Moderna shared data from its phase 1/2 trial of its avian flu vaccine, showing that three weeks after the second dose, nearly 98% of participants reached antibody levels considered protective. In a statement, Bancel wrote: “While the termination of funding from HHS adds uncertainty [ . . . ] we will explore alternative paths forward for the program.”
The scientific community’s reaction to HHS’s moves has ranged from befuddlement to outrage. “This MAHA approach to killing vaccine technologies for ideological reasons and nothing to do with vaccines is both foolish and deadly. It weakens our nation’s biosecurity,” says Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine, codirector of Texas Children’s Hospital Center for Vaccine Development, and codeveloper of the low-cost COVID vaccine Corbevax. “It also reinforces my view that the MAHA movement is little more than an economic stimulus for the very corrupt wellness and influencer industry. We learned both from Ebola in Democratic Republic of Congo and COVID-19 that the single most important lesson of pandemic preparedness is to keep many vaccine technologies in play, because you cannot predict ahead of time which ones might rise to the top.”
There are currently three licensed H5N1 vaccines (made by GSK, CSL Seqirus, and Sanofi) that are either made in eggs or grown in cell culture. None are commercially available, though the government has been adding to its stockpile. Even so, getting an up-to-date version of these vaccines ready for broad distribution would take many months. An mRNA-based vaccine, in contrast, could be matched to the most recently circulated variant of the virus and manufactured rapidly.
Other drugmakers, including GSK-Curevac and Pfizer, have been working on mRNA vaccines for avian flu. It’s unclear what will happen to these programs now. Joe Payne, CEO of San Diego-based Arcturus Therapeutics, says that his company continues to have “full support” from the Biomedical Advanced Research and Development Authority (BARDA), which has committed up to $63 million to help advance the company’s avian flu vaccine. (Arcturus’s version uses self-amplifying mRNA, a new technology that works at lower doses than first-generation mRNA vaccines like Moderna’s.) This April, Arcturus received FDA Fast Track designation for the vaccine, which is currently being tested in a phase 1 trial.
Arcturus has also developed a self-amplifying mRNA COVID vaccine with CSL Seqirus, which the companies aim to submit for FDA approval later this year. “There’s been a desire in the scientific community and regulatory agencies to identify lower-dose alternatives,” says Payne. The new FDA guidance, he says, “is a positive development for us, because it’s a fair, balanced and professional communication on their COVID policy, where a couple months ago [under Trump], there was a lot of uncertainty.”
mRNA in the MAHA crosshairs
The long-term bet on Moderna rides almost entirely on its individualized cancer therapy, mRNA-4157, which it’s developing in conjunction with Merck. While sometimes called a personal cancer vaccine, mRNA-4157 doesn’t actually protect you from getting cancer, but instead trains the immune system to attack an existing tumor, using custom-made mRNA that encodes antigens specific to each person’s cancer.
The company has high hopes that the therapy can be used to treat multiple kinds of cancers. In Phase 2 trials, the therapy cut the risk of recurrence or death in advanced melanoma (after surgical resection) by 65% when combined with Merck’s drug Keytruda, compared with Keytruda alone. Moderna also has trials underway or enrolling for its use in treating high-risk melanoma, non-small cell lung cancer, invasive bladder cancer, and adjuvant renal cell carcinoma.
While these personalized treatments could be very lucrative for the company, they won’t be easy to scale quickly. And the timeline for FDA approval is uncertain, depending on trial results and regulatory review. The melanoma study isn’t expected to be fully complete until 2030, and the FDA has not been supportive of accelerated approval. Whether Moderna can hang on that long is an open question.
In the meantime, a host of researchers and well-funded biotechs developing second- and third-generation therapies using mRNA and related technologies are quietly holding their breath, feeling that, for now, Kennedy and his lieutenants are concerned almost exclusively with examining the use of mRNA in protective vaccines for healthy people. Using mRNA for treating cancer and rare diseases seems to be a different story.
In the past year or so, researchers at the University of Florida and Memorial Sloan Kettering have published promising results from small studies of personalized mRNA-based therapeutic vaccines for glioblastoma and pancreatic cancer, respectively. “The next wave of mRNA is with inhaled mRNA and intravenously dosed mRNA to treat really serious and fatal rare disease conditions,” says Payne at Arcturus. “And that’s where we’re getting the warmest support from the new administration.”
“There is a general belief that science will prevail,” says another CEO of a venture-backed company focusing on therapeutic uses of self-amplifying mRNA. “But there is anxiety from the uncertainty. Uncertainty is not good for anything.”
Perhaps no company knows that better than Moderna.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0
.jpeg?width=1200&auto=webp&trim=0,0,0,0#)