Why urban designers should think like doctors
What if buildings and neighborhoods were planned with health and climate risks in mind, just like businesses use financial data to guide their decisions? What if public health and real estate weren’t at odds, but instead coauthors of a healthier, more equitable urban future?
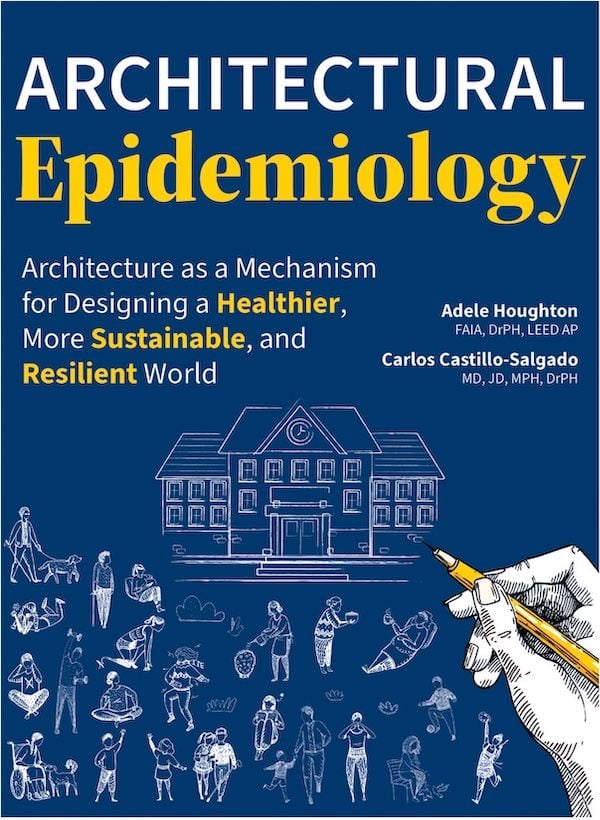
That’s the bold premise of Architectural Epidemiology, a new book that offers a radical rethinking of the relationship between place and health. Written by architect and public health expert Adele Houghton and Dr. Carlos Castillo-Salgado, an epidemiologist, the book introduces a place-based framework for aligning real estate investment with public health goals—using the tools of epidemiology to guide design decisions that affect buildings and the way they engage the surrounding city.
At its core, architectural epidemiology is not a metaphor. It’s a methodology.
Diagnosing places like patients
Just as a doctor might diagnose a patient based on symptoms and environmental exposures, Houghton and Castillo-Salgado’s framework helps designers, developers, and policymakers diagnose the health of a place.
The process begins by gathering publicly available health and climate data—rates of asthma, heat exposure, housing-cost burden, chronic illness, and more—and dialing into the specific needs of any real estate project boundary. These place-based insights then inform customized development strategies tailored to local needs.
This isn’t a one-size-fits-all checklist. It’s a locally calibrated, equity-centered approach that asks: What are the most urgent public health and climate concerns in this neighborhood? And how can this project become part of the solution?
Two case studies from the book, one in the South Bronx and another in East London, show how this approach plays out in the real world.
Toxic infrastructure to health-first housing
The South Bronx is one of New York City’s most environmentally burdened neighborhoods. Residents face compounding public health concerns, including high rates of obesity, diabetes, heart disease, and pediatric asthma—conditions tied directly to chronic exposure to air pollution, extreme heat, and poor housing conditions. Infrastructure like solid waste transfer stations, natural gas plants, and a daily flow of more than 750 diesel trucks has left a lasting environmental footprint.
Three projects demonstrate how health-driven interventions play out in real life.
Arbor House, a 124-unit LEED Platinum affordable housing development, took an indoor-focused strategy. With no regulatory leverage to reduce nearby traffic or emissions, the project team instead designed a protective shell: a high-performance building envelope, mechanical exhaust and ventilation systems, low-VOC materials, and a no-smoking policy. These features directly addressed local respiratory and cardiovascular risk data, providing a sanctuary of clean air in a polluted context.
The Eltona, another LEED Platinum project by the same developer, built on these strategies but also benefited from its location within the Melrose Commons urban renewal zone. This area, guided by a community-authored plan, introduced pedestrian-prioritized streets and small green spaces to break up heat and pollution hot spots. This sort of coordinated planning can push health equity beyond the building envelope.
The Peninsula represents an even bolder intervention: transforming a former juvenile detention center into a mixed-use anchor of community well-being. Once all phases are complete (anticipated in 2026), the project will deliver 740 units of affordable housing, a wellness center, daycare, supermarket, light industrial space, and a workforce development hub—all aligned with the long-standing Hunts Point Vision Plan. Created through a collaborative effort between local government and community groups, the plan calls for cleaner air, economic opportunity, and access to green space without displacing existing residents.
This multiscalar transformation wouldn’t have been possible without partnership. The development team committed to providing both affordable and middle-income housing, as well as commercial and industrial spaces aligned with local needs. The local government played a convening role, confronting outdated zoning and building codes to enable community-led regeneration. And community groups acted as watchdogs and visionaries—documenting health inequities, advocating for residents’ needs, and ensuring decades of disinvestment didn’t translate into displacement.
From industrial blight to inclusive growth
In East London’s Hackney borough, Gillett Square shows how long-term, community-led urban design can build resilience without triggering displacement. Residents here also face elevated risks from exposure to traffic-related air pollution, unsafe pedestrian conditions, and mental health stressors, particularly among children and the elderly. Climate concerns such as extreme temperatures compound vulnerability, especially in a borough with high poverty rates and a large renter population.
The project began in the 1980s as part of a broader, three-pronged effort to reduce crime, create economic opportunity for women- and minority-owned businesses, and preserve affordability in the face of rapidly rising property values. Organized by Hackney Co-operative Developments, a community interest company, this initiative has grown over 40 years into a model of place-based health equity.
Unlike top-down redevelopment, the transformation of Gillett Square unfolded through continuous negotiation among residents, developers, and the local government. A former parking lot became the square itself. Adjacent buildings were renovated to create 30 affordable workspaces and 10 retail units prioritized for local startups and cultural groups. The existing street-facing storefronts remained intact, maintaining the character and economic rhythms of the block. During construction, current tenants were temporarily relocated—but not displaced—a rare feat in most urban redevelopment narratives.
The built environment improvements weren’t just aesthetic or economic. The renovated Bradbury Works building added insulation, operable windows, and improved ventilation to respond to extreme temperatures and indoor air quality concerns. It was also designed to accommodate a future rooftop solar array.
Elsewhere on the square, an old factory became a jazz club. Another was converted into a mixed-use building with social housing and office space. Each adaptive reuse project layered with health-promoting elements such as natural light, passive ventilation, and energy efficiency.
Importantly, these design moves responded to both immediate and long-term public health concerns identified in the architectural epidemiology framework: exposure to air pollution, heat vulnerability, mental health stressors, and pedestrian safety risks.
The health situation analysis for the neighborhood emphasized the need for strategies that reduced the risk of obesity, mental health issues, and traffic-related injury, many of which were tackled by fine-grained, community-rooted design rather than by sweeping interventions.
Gillett Square’s evolution also depended on progressive land use policy and community engagement over time. The local government enabled critical rezonings: converting the parking lot into a plaza, allowing mixed-use development, and permitting the installation of small retail kiosks. The development team, operating as a nonprofit social enterprise, prioritized community interests. And community groups, many of which had been active in Hackney for decades, fought to ensure that the square’s benefits didn’t come at the expense of its existing residents.
In a borough where 75% of residents are renters, and poverty rates among children and the elderly are among the highest in the U.K., the stakes of gentrification are high. Gillett Square proves that design can support resilience without fueling displacement—and that longevity, not speed, can be a hallmark of justice-oriented urban development.
These case studies show that health equity can be the foundation, not a by-product, of urban development. By aligning investments with public health and climate data, Architectural Epidemiology offers a road map for building places that protect and uplift communities. This framework identifies community needs and guides community residents, developers, and designers to solutions that create value for both stakeholders and shareholders.
This story was originally published by Next City, a nonprofit news outlet covering solutions for equitable cities. Sign up for Next City’s newsletter for the latest articles and events.
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0